Want to write a piece for 3DHEALS Expert Corner? Email us: info@3dheals.com
Over the past decade, there has been an exponential increase in the utilization of 3D printing technologies for cardiovascular applications. 3D printing is being utilized in many cardiovascular centers of excellence for surgical planning and simulation, trainee education and patient counseling.
I. Surgical planning and pre-procedural simulation
To attain the best surgical outcomes, cardiac surgeons need to operate efficiently and obtain the best possible surgical result on their first attempt. This requires a keen understanding of complex three-dimensional anatomy, a high level of technical skill, and the ability to make critical decisions in a short amount of time. Each of these factors is enhanced by 3D printing.
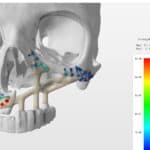
Currently, the standard of care requires surgeons to mentally reconstruct complex 3D anatomy from stacks or sweeps of 2-dimensional images; echocardiograms, MRIs or CTs. “3D” volume rendered images go a step further to show spatial relationships, but are limited by the 2D displays on which they are usually shown. On the other hand, 3D-printed models are replicas of the patient’s own unique anatomy that a surgeon can hold, manipulate and obtain a very detailed understanding of complex anatomy. Examples are shown in Figure 1.

When printed in flexible and compliant materials, surgeons can cut, suture and engraft patches, conduits, and essentially perform a simulated surgery before stepping into the operating room. In so doing, surgeons effectively get a “practice swing” before performing the actual surgery. This type of precise pre-surgical planning potentially offers several benefits:
- Reductions in procedure time, which has been linked to improved surgical outcomes.
- Planning for contingencies (Plan A, Plan B, etc) and “bailout” strategies
- Fewer residual lesions and decreased re-intervention rate
- Shorter post-operative hospital stays given the relatively recent growth of cardiac 3D printing to date there have been no long-term studies to date confirming the potential benefits above. However, clinical utilization is growing, and several papers have reported promising applications of the technology (1-8). In addition, early data from the otolaryngology experience is showing reductions in procedure time (9-10).
II. Trainee Education
There is an often quoted idiom in medical education: “See one, Do one, Teach one.” This refers to a model of medical training that has persisted as long as the medical profession itself; an apprenticeship model whereby medical trainees learn from the observation and teachings of more experienced clinicians.
In the method, teaching is both didactic and experiential, essentially learning through experience in live cases. Our greatest surgeons have trained in this method, and over time they have accumulated a high degree of skill after performing large numbers of cases and committing thousands of hours of practice. At the same time, further examination of this model of medical education makes plain some of its drawbacks:
- It is highly dependent on the availability of teaching cases – both the number of cases and a wide variety of complexity required to provide a solid training experience
- Variability of teaching skill and experience of the educator
- Learning via practice on actual patients. This last point is particularly noteworthy; it is an inescapable reality of the current medical system, which has overall worked well for generations, though not particularly comforting to patients or their families. 3D printing technologies provide solutions that enhance trainee education to overcome some of the limitations above5. 3D printed models that represent the spectrum of complex cardiovascular abnormalities can be made for trainees to perform difficult procedures, limited only by their access to the technology. This helps transition from solely an apprenticeship model to a “simulator-based” learning model that has already made other industries safer. As an example, consider the airline industry and training with flight simulators. With 3D printed models we can now provide the next generation of trainees the “1000 hours” (or more) of practice they need performing complex procedures. This new approach augments current education methods and standardizes the ways in which future heart surgeons are trained, hopefully producing surgeons who are better prepared to operate on live patients.
III. Patient and Family Counseling
One of the bedrocks of the practice of medicine is the cultivation and practice of empathy. Empathy is what allows us to put ourselves in our patient’s shoes and imagine their medical experience from their perspectives. It is what helps us connect with the families we serve and ultimately work as a team to tackle medical problems. To that end I invite you to engage in this thought exercise: imagine being a patient, or the parent of a young child, who is learning a complex diagnosis for the first time. Then imagine having to make difficult and complicated decisions regarding this diagnosis, which may involve high-risk surgery. These are the types of situations our patients and families face on a daily basis, and the process of patient and family counseling is fraught with challenges. Some of these challenges have to do with the complexity of the disease, which may interfere with the patient’s ability to make informed decisions about medical or surgical options. For cardiac cases, 3D printed models allow the patient to hold a replica of their own heart while his/her physician goes over their diagnosis, treatment options, and the planned procedure. Just as it was for experienced surgeons and trainees, 3D models offer the patient a higher level of understanding of their own anatomy, hopefully enhancing the informed consent process, and helping patients and families make better decisions (11-12).
IV. Future Directions & Transformative Partnerships
While cardiac applications of 3D printing have advanced far in the past decade, the next few years promise to be even more exciting. 3D printing will help push the envelope of personalized medicine, opening up possibilities that were simply unavailable in the past without this technology. One example is cardiac bioprinting, which will allow the engraftment of patient-matched 3D printed cardiac structures (valves, vessels, myocardium, etc) (13-14). Other advanced applications include 3D printing for functional 3D modeling, which allows physicians to integrate physiology into 3D models and predict the outcomes of surgeries. Finally, it is very likely that 3D printing using biocompatible materials will be applied to develop the next generation of cardiac implants and devices. 3D printed implants are now routinely used in non- cardiac specialties (ex: orthopedics, craniofacial, dentistry), and the technology is ready for adoption for cardiac applications. These advanced implants will overcome the limitations of currently available products and further improve surgical outcomes.
To achieve the next generation of breakthroughs, new transformative partnerships will be essential. The rapid evolution and complexity of this technology makes collaboration essential for the stakeholder sectors; academic, medical, and commercial. These transformative and synergistic partnerships will undoubtedly elevate patient care and result in improved medical outcomes in the near future.
Disclosure: Dr. Anwar is a Consultant at Printerprezz, a medical innovation company utilizing additive manufacturing, nanotechnologies, and surgical expertise to design and manufacture next-generation medical devices based in Fremont, CA.
References:
1. Anwar, S et al. 3D Printing in Complex Congenital Heart Disease: Across a Spectrum of Age, Pathology, and Imaging Techniques. JACC: CV Imaging. 2016. http://doi.org/10.1016/j.jcmg.2016.03.013
2. Farooqi, et al. Application of Virtual3D Models for Simultaneous Visualization of Intracardiac Anatomic Relationships in Double Outlet Right Ventricle. Pediatr Cardiol. 2015 Aug 9;37(1):90–8.
3. Farooqi, et al. 3D Printing to Guide Ventricular Assist Device Placement in Adults With Congenital Heart Disease and Heart Failure. JACC: Heart Failure. 2016, 4(4), 301–311.
4. Ryan JR , et al. A novel approach to neonatal management of tetralogy of Fallot, with pulmonary atresia, and multiple aortopulmonary collaterals. JACC: CV Imaging. 2015 Jan 1;8(1):103–4.
5. Costello, et al. Incorporating 3D Printing into a Simulation‐based Congenital Heart Disease and Critical Care Training Curriculum for Resident Physicians. Congenital Heart Disease. 2015 Mar 1;10(2):185
6. Anwar, S., Singh, G. K., Miller, J., Sharma, M., Manning, P., Billadello, J. J., et al. (2018). 3D Printing is a Transformative Technology in Congenital Heart Disease. JACC: Basic to Translational Science, 3(2), 294–312. http://doi.org/10.1016/j.jacbts.2017.10.003
7. Tack, P., Victor, J., Gemmel, P., & Annemans, L. (2016). 3D-printing techniques in a medical setting: a systematic literature review. BioMedical Engineering OnLine, 1–21. http://doi.org/10.1186/s12938-016-0236-4
8. Byrne, N., Velasco Forte, M., Tandon, A., Valverde, I., & Hussain, T. (2016). A systematic review of image segmentation methodology, used in the additive manufacture of patient-specific 3D printed models of the cardiovascular system. JRSM Cardiovascular Disease, 5, 2048004016645467.http://doi.org/10.1177/2048004016645467
9. Zweifel DF, Simon C, Hoarau R, Pasche P, Broome M Are Virtual Planning and Guided Surgery for Head and Neck Reconstruction Economically Viable? Journal of Oral and Maxillofacial Surgery 2015
10. Rogers-Vizena, C. R., Sporn, S. F., Daniels, K. M., Padwa, B. L., & Weinstock, P. Cost-Benefit Analysis of Three-Dimensional Craniofacial Models for Midfacial Distraction: A Pilot Study. The Cleft Palate-Craniofacial Journal. 2017.
11. Hu A, et al. Three-dimensional Educational Computer Model of the Larynx: Voicing a New Direction. Arch Otolaryngol Head Neck Surg. American Medical Association; 2009.
12. Bernhard, J. et al. Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World Journal of Urology, 2016.
13. Bin Duan. State-of-the-Art Review of 3D Bioprinting for Cardiovascular Tissue Engineering. Annals of Biomedical Engineering. Springer US; 2016 Aug 18;1–15
14. Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 3D Printing of Personalized Thick and Perfusable Cardiac Patches and Hearts. Advanced Science. John Wiley & Sons, Ltd; 2019 Apr 15;135:1900344.
About the Author
 Dr. Shafkat Anwar is a pediatric cardiologist with a specialty in non-invasive cardiac imaging, including echocardiography and cardiac magnetic resonance imaging (MRI).
Dr. Shafkat Anwar is a pediatric cardiologist with a specialty in non-invasive cardiac imaging, including echocardiography and cardiac magnetic resonance imaging (MRI).
He is the Pediatric Cardiology Director of Cardiac MRI, as well as Co-Founder and Co-Director of the UCSF Center for Advanced 3D+ Technologies (CA3D+). He is a founding member and the inaugural Chair of the Advanced 3D+ Visualization Special Interest Group in the Society for Cardiovascular Magnetic Resonance. He is a consultant at Printerprezz, a medical start-up in Fremont, CA utilizing additive and other advanced manufacturing technologies to develop the next generation of medical devices. At Printerprezz Dr. Anwar serves as the Senior Vice President of Medical Innovations. Dr. Anwar completed his internship and residency in Pediatrics at Children’s National Medical Center, as well as a research fellowship at the National Institutes of Health. He completed fellowships in Pediatric Cardiology and Cardiac Imaging at Cleveland Clinic and Children’s Hospital of Philadelphia. Prior to joining UCSF, Dr. Anwar was Cardiology Director of Cardiac MRI at Washington University in St. Louis, St. Louis Children’s Hospital. At Wash. U. Dr. Anwar co-founded and co-directed the Center for 3D Printing, a multi-disciplinary 3D printing center
Related Articles:
From 3D Printing to VR/AR: Simple Connection?
Interview: Justin Ryan, 500+ Heart Models later…
Interview: Dr. Sujatha Buddhe, Pediatric 3D Printing, Seattle
Interview: Dr. Chen Ching Kit, Pediatric Cardiac 3D Printing, Singapore
Idea to Implementation: Revenue Strategies for 3D Printing for Pre-surgical Planning




 Jun 01, 2019
Jun 01, 2019 





Comments